Deep Sclerectomy Surgery in the U.S.
Deep Sclerectomy is a highly effective, non-penetrating glaucoma surgery designed to lower intraocular pressure (IOP) while minimizing complications. By creating a new drainage pathway in the outer layers of the eye (sclera), this procedure allows fluid (aqueous humor) to flow out more efficiently, preventing optic nerve damage and preserving vision.
Unlike a trabeculectomy, which fully opens the eye’s drainage pathway, deep sclerectomy leaves a thin layer of tissue intact, reducing the risk of sudden drops in eye pressure and postoperative complications.
Why Deep Sclerectomy Is Recommended
Ophthalmologists recommend deep sclerectomy surgery for patients with open-angle glaucoma who:
-
Have not achieved target IOP despite maximum tolerated medications
-
Require a safer alternative to full-thickness glaucoma surgery
-
Are at higher risk of complications from trabeculectomy or tube shunt procedures
This procedure is preferred in cases where gradual and controlled pressure reduction is needed, particularly for patients with moderate to advanced glaucoma.
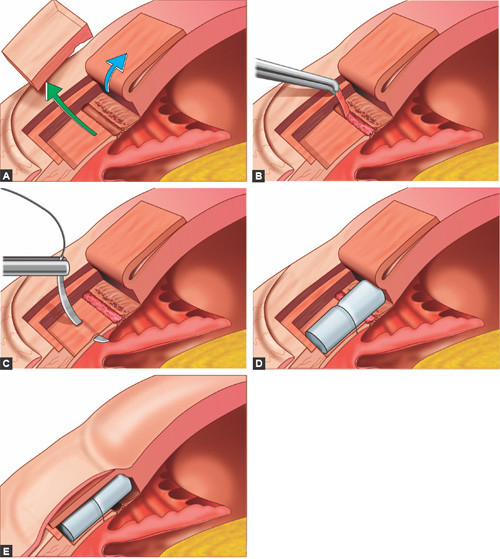
How the Procedure Works
During deep sclerectomy, the surgeon removes a deep layer of scleral tissue, leaving a thin layer of trabeculo-Descemet’s membrane. This creates a controlled filtration space where fluid can percolate through and collect under the conjunctiva, forming a “bleb.”
Key points about the procedure:
-
Anesthesia: Usually performed under local or regional anesthesia.
-
Duration: Around 30–45 minutes per eye.
-
Hospital Stay: Typically outpatient; patients go home the same day.
-
Adjuncts: Implants such as collagen, hyaluronic acid spacers, or antimetabolites (like mitomycin C) may be used to prevent scarring and improve long-term success.
Patient Selection Criteria
Not all glaucoma patients are candidates for deep sclerectomy. Ideal candidates usually have:
-
Primary open-angle glaucoma
-
Pseudoexfoliative or pigmentary glaucoma (early to moderate stages)
-
Good conjunctival health for bleb formation
-
No extensive angle closure or previous scarring that would prevent proper filtration
Patients with advanced scarring, severe neovascular glaucoma, or previous failed filtration surgeries may be advised to consider alternative procedures such as trabeculectomy or glaucoma drainage implants.
Advantages of Deep Sclerectomy
-
Lower Risk of Complications – Less chance of hypotony, infection, or bleb leaks compared to trabeculectomy.
-
Stable Pressure Control – Provides consistent and gradual IOP reduction.
-
Faster Recovery – Reduced inflammation and quicker return to daily activities.
-
Customizable Procedure – Can be combined with implants or antimetabolites to enhance long-term success.
-
Repeatable if Needed – The procedure can sometimes be revised if filtration decreases over time.
Risks and Complications
Although safer than more invasive procedures, deep sclerectomy surgery may still have risks:
-
Scarring of the filtration site, reducing effectiveness over time
-
Mild postoperative discomfort or blurred vision
-
Over-filtration (rare), which can lead to low IOP
-
Need for postoperative laser goniopuncture to improve flow through the remaining tissue
Regular follow-up visits are crucial to ensure the filtration space remains functional and pressure remains controlled.
Recovery and Postoperative Care
Recovery from deep sclerectomy is typically faster than from trabeculectomy, but careful follow-up is still required.
Typical recovery timeline:
-
First few days: Mild redness and discomfort; eye drops prescribed.
-
First month: Gradual stabilization of IOP; bleb is monitored closely.
-
1–3 months: Most patients resume normal activities; pressure readings are adjusted as needed.
Patients are advised to avoid strenuous activities, eye rubbing, and heavy lifting during the early recovery phase.
Success Rates and Long-Term Outcomes
Clinical studies show that deep sclerectomy can lower IOP by 30–50% on average. Success rates are high, particularly when combined with antimetabolites or implants. Long-term studies indicate that many patients remain medication-free for several years after surgery, though some may eventually need additional treatment.
Comparison with Other Glaucoma Surgeries
| Surgery Type | Invasiveness | IOP Reduction | Risk Level | Recovery Time |
|---|---|---|---|---|
| Deep Sclerectomy | Moderate | High | Lower Risk | Shorter |
| Trabeculectomy | High | Very High | Higher Risk | Longer |
| Tube Shunt Surgery | High | High | Moderate | Moderate |
| Laser Treatments | Low | Mild-Moderate | Low | Minimal |
Deep sclerectomy strikes a balance between safety and effectiveness, making it an excellent choice for many glaucoma patients.
Availability in the Philippines
In the Philippines, deep sclerectomy may not be as widely available as in the U.S. It is typically performed in advanced eye centers or large hospitals with glaucoma specialists. Patients considering this surgery locally should consult an ophthalmologist to confirm availability and discuss whether they are suitable candidates.
Cost of Deep Sclerectomy in the U.S.
The cost of deep sclerectomy surgery in the U.S. usually ranges between $3,000 and $5,000 per eye, depending on the facility, surgeon, and use of implants or adjunctive medications. Insurance may cover a significant portion of the cost if the procedure is medically necessary.